By Jessica Haynes, OD


Meeting a new patient who doesn’t yet have AMD-related vision loss makes for a great clinic day. And sometimes (although not as often as I would like) I get to see choroidal neovascularization (CNV) patients who present with 20/20 vision. When this happens, I’m so grateful to the referring doctor because I believe we can make a big difference in that patient’s quality of life. The million-dollar question is: How can all primary care optometrists help make these timely referrals the norm rather than the exception?
One challenge in primary eye care is lack of access to the range of tools needed to make fully-informed decisions that help guide early intervention and prompt referrals. That makes it really hard. None of us want to rely on what we think instead of what we know—especially when we’re treating a potentially blinding disease. Yet this is often the reality.
If your practice has access to technologies such as OCT, FAF, OCT-A, and dark adaptation (commercially available as AdaptDx by MacuLogix), you have a much more reliable compass to help navigate decision-making, and it’s a lot easier to decide whether it’s time for vitamin supplementation, home monitoring devices such as Notal Vision’s ForeseeHome system, or for a referral to a retinal specialist. Each of these tools provides unique insight into the disease. In combination, they paint a more complete picture of AMD, allowing us to better identify who is at higher risk of conversion to advanced stage disease, and detect that conversion earlier. Without these tools, we have to rely exclusively on what we can see—and although careful fundus evaluation remains crucial, ancillary testing allows us to see what’s happening beneath the surface and alert us to clinically unseen threats to vision.
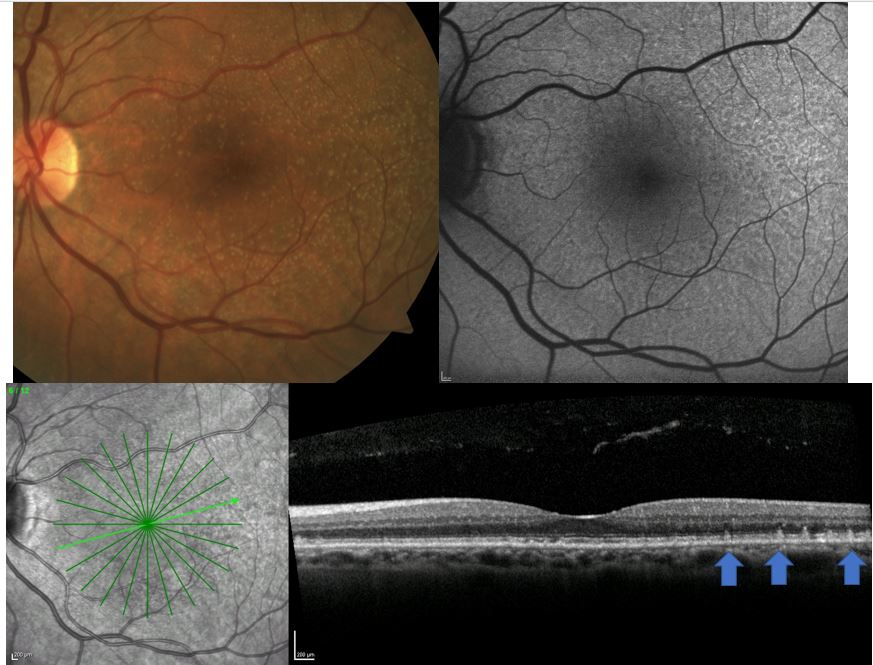
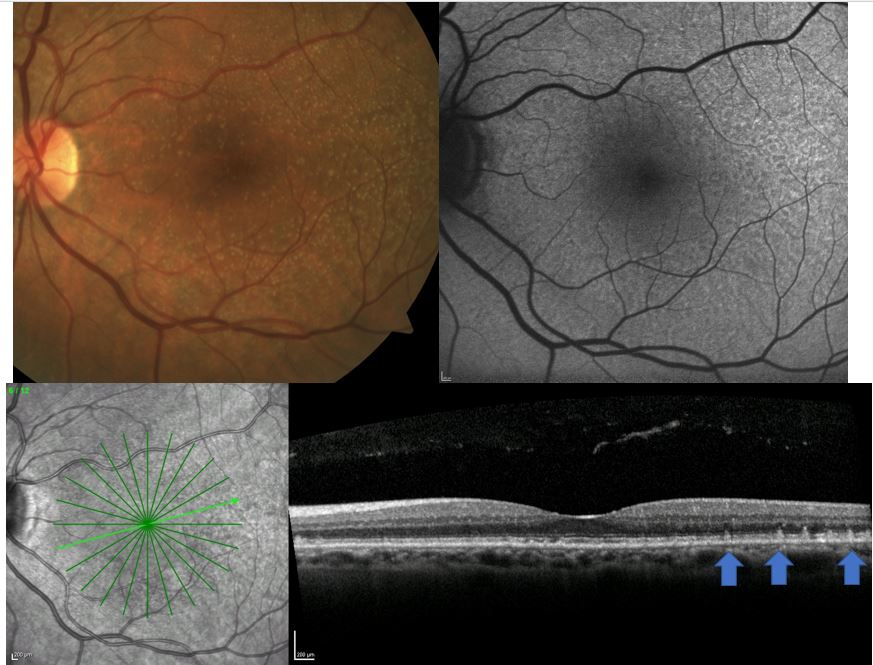
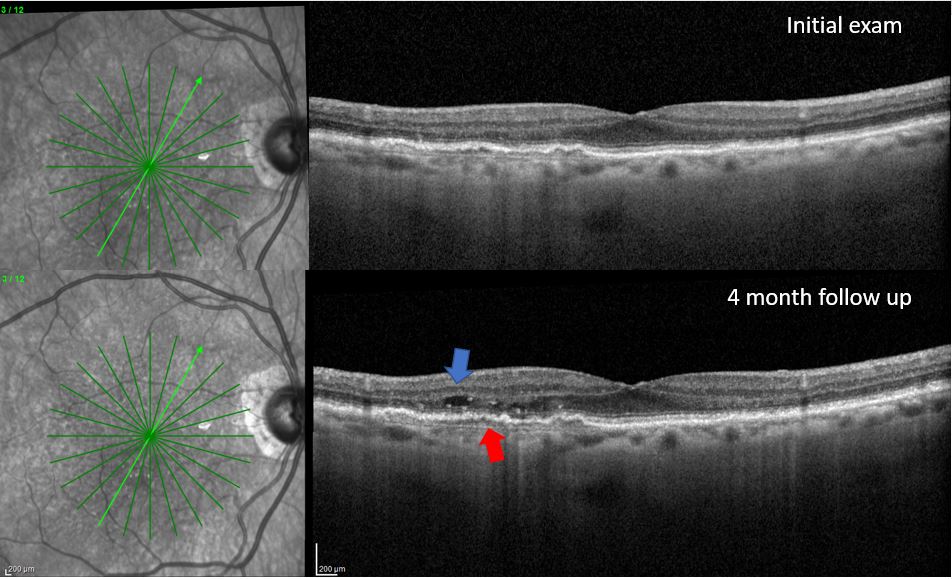
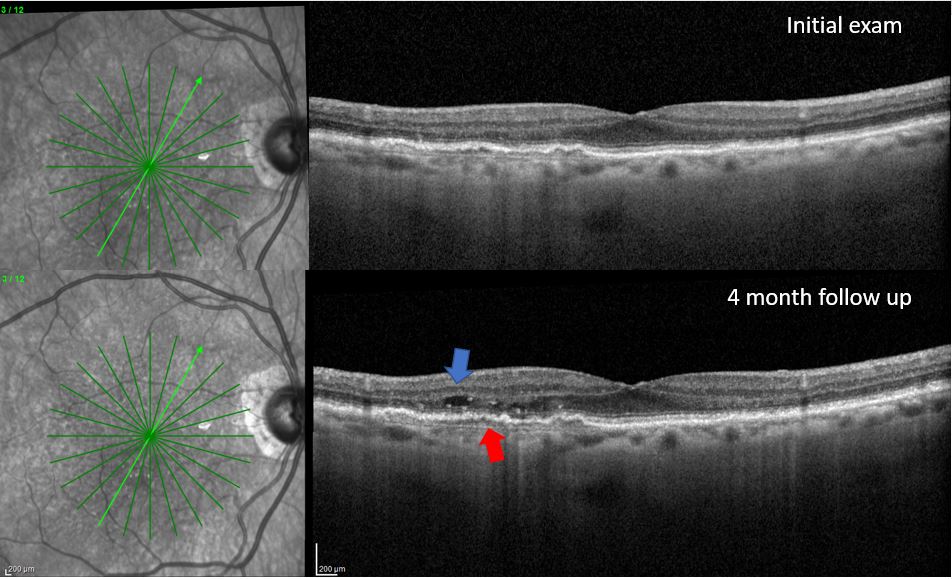
In our clinic, I get a baseline OCT and FAF on every patient, which helps me detect disease that can’t be seen clinically (Figure 1 and 2). These tools alongside dark adaptation in the primary care setting, may alert the primary care optometrist of a more advanced disease process than is clinically visible.
Indeed, I am encouraged that there seems to be a trend toward increased adoption of these technologies, and, with that in mind, I would recommend that my colleagues make as much use of them as possible because they really can make a big difference for our patients. The key is in putting everything together. If you don’t see any drusen, but a dark adaptation evaluation reveals a problem, you know you should run an OCT to evaluate more carefully the outer retina, retinal pigment epithelium and choroid. This becomes a very easy decision. If the OCT is abnormal, it’s potentially time to start considering supplements and perhaps even prescribe the ForeseeHome system if there is evidence of intermediate stage AMD.
If the OCT is normal, care should still be taken to advise these patients about important lifestyle modifications to reduce their risk of developing clinically visible AMD, and ultimately reduce their risk of vision loss from AMD. Testing should be looked at comprehensively to paint a bigger picture of the disease. This is a thoughtful and medically oriented approach to optometric practice. Each test informs the next and all of them combined dictate the recommendation we make to the patient.
There is no need to alarm patients nor to give them a false sense of security. Both of these scenarios are equally inadvisable. Indeed, the way to proceed with real confidence when managing patients who have not yet progressed to a stage with compromised vision is to take all the pieces of the puzzle—the OCT, FAF, OCT-A, dark adaptation and the fundus evaluation—and base your strategy on this more complete dataset.
Dr. Haynes is in practice at the Charles Retina Institute in Germantown, Tennessee.



