

By Anne-Marie Lahr, OD
When you do something long enough, you get very comfortable. You know it inside and out. That’s how I felt for many of
the 24 years I spent educating others about ophthalmic optics and lens design. Despite my years involved in all things eye care-related, from academics to industry, I recently discovered that I still have much to learn in this constantly evolving field. When I joined MacuLogix as the associate director of professional relations, it was immediately clear that I would need to review and reacquaint myself with the anatomy and physiology of the retina to understand the progression of age-related macular degeneration (AMD).
Never stop learning
The quote, “Never stop learning because life never stops teaching,” ties into my overall approach to life and recent experiences. I quickly became aware that what we know about the retina and macula has evolved over that past 20 years. Here are my key takeaways as I dove into the research and rediscovered the retina:
1) Rods outnumber cones in the macula. Sometimes eye care professionals think in generalities, recalling the rods are found in the periphery and cones dominate the macular area. However, rods actually outnumber cones in the macula—in fact, there are nine rods for every cone. Of course, the fovea is cone-dominated, but the larger parafovea is rod-dominated.
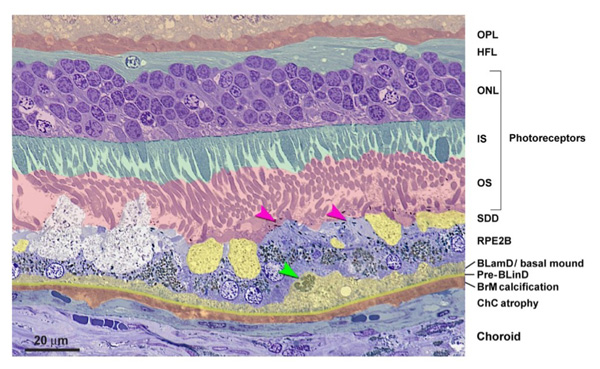
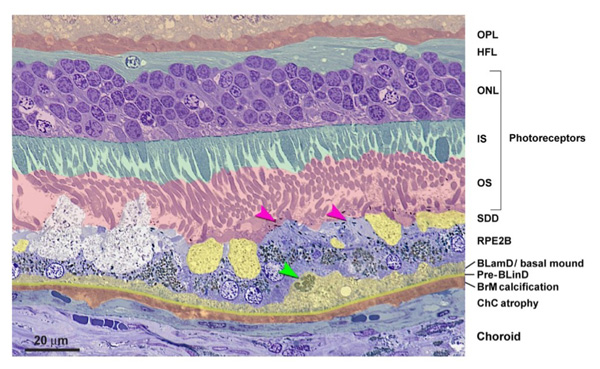
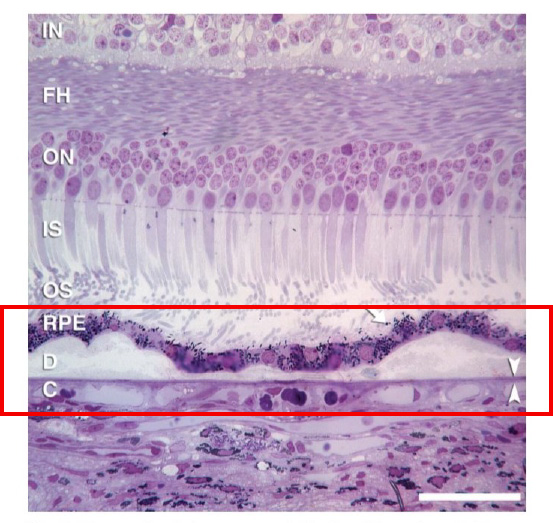
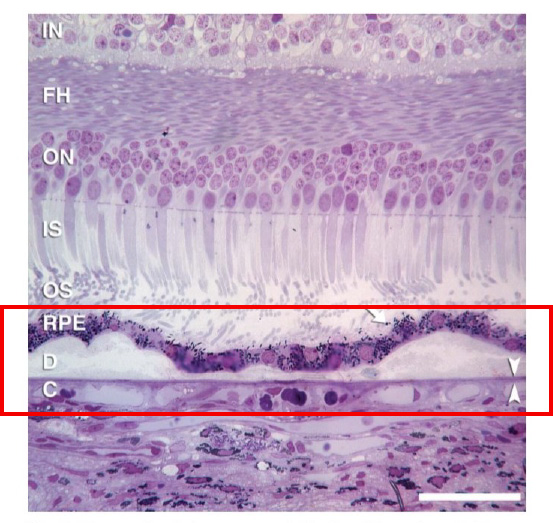
2) It’s a misconception that visible drusen are the primary lesions in AMD. In fact, the primary lesions associated with AMD occur within Bruch’s membrane and the retinal pigment epithelium (RPE). These lesions are not visible with clinical imaging or research imaging in vivo.
3) The primary lesions in AMD are made of cholesterol—the same type that is found in the arteries of those with atherosclerosis. The morphology of the lesions is the same in the two diseases. The panmacular cholesterol—or more specifically, basal laminar and basal linear deposits (BLamD and BLimD, respectively)—accumulates in Bruch’s membrane and between the basal surface of the RPE cells and Bruch’s membrane.
4) Drusen are all connected. Visible drusen are just the tip of the iceberg. Histopathological studies show that drusen are an accumulation of the panmacular cholesterol deposits. As the cholesterol builds up, drusen become clinically visible. Even though they appear as individual spots on the macula, they are just peaks of the invisible cholesterol layer. Just like an iceberg lurking under the water, there are plenty more drusen below what can be seen on the surface.
5) Night blindness is the first symptom of AMD. Cholesterol deposits cause localized vitamin A deficiency that leads to impaired night vision. These lesions of cholesterol cause Bruch’s membrane to thicken, creating oxidative stress and inflammation that impedes the normal transport of nutrients from the choriocapillaris, including that of vitamin A. That, in turn, affects photoreceptor health and creates a localized vitamin A deficiency.
Research shows that dark adaptation function is compromised from the earliest stages of AMD, and impairment increases as the disease progresses. In fact, impaired dark adaptation indicates the presence of AMD at least three years before drusen are visible upon clinical examination, making dark adaptation the canary in the coal mine for the detection of AMD. By understanding impaired dark adaptation and its connection to AMD, we will be much better equipped to tackle this progressive eye disease.
Be a trailblazer
These five takeaways are the cornerstones to understanding the retina and how it relates to AMD. Although this was knowledge I had already obtained, I had to brush up on it to sharpen my skills as I took on this new leadership position. Open yourself up to learning something new. Education truly is the key to being a trailblazer.
About the Author
Prior to her role with MacuLogix as associate director of professional relations, Anne-Marie Lahr, OD, spent 23 years educating others about ophthalmic optics and lens design at Salus University and Hoya Vision Care. She has a width breadth of clinical eye care knowledge in research, medical devices, strategic planning and much more. Dr. Lahr earned her OD degree at the Ohio State University College of Optometry.



