This story was originally printed in our June 2011 issue
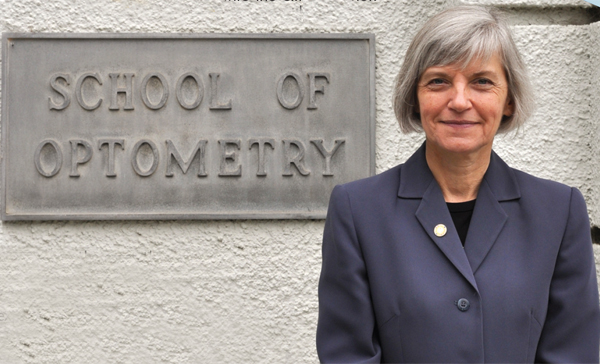
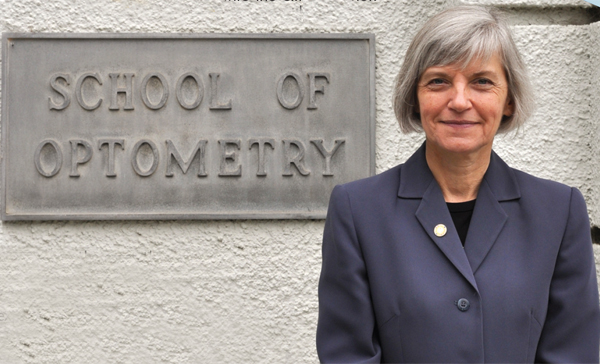
When Pia Hoenig, OD, MA, DBO(T), FAAO, chief of the Binocular Vision Clinic at University of California, Berkeley, was approached by a group of second-year optometry students who wanted to gain additional clinic experience, she thought it was a great idea. It would benefit her to expose students to children’s vision and the neuro-optometric specialty earlier, and it would provide students with a chance to gain important perspective.
As a result, students now have their first dose of rotations through this tertiary eye care clinic—which sees children with binocular vision issues as well as more complex cases of children with significant learning challenges, mild traumatic head injuries, strokes and other neurological problems—in their second year.
This academic year, the earlier clinical rotations became a part of the established curriculum, and the idea grew from that first student-initiated request made three years ago. Dr. Hoenig says not only may it help clinic patients, it definitely adds value to the educational experience. “If you’re going to survive in private practice and offer specialty/tertiary eye care services, you need to know what you’re doing. You need to have clinical exposure, not just academic knowledge from class.”
Here’s how the tiered approach works now.


All second-year students sign up to work two short rotations in the binocular vision clinic, once at the beginning of the semester and once toward the end. Dr. Hoenig takes four or five students at a time and they focus on one particular patient. “We prep the chart together, see the patient, enter the data in the electronic medical record and work on the write-up together.”
All third-year students rotate through the clinic two full days in a two-month period. “We work in groups of two or three, and students have a chance to prep ahead of time. They’ll know who the patients of the day are, and we hold a seminar where they come in and report on those patients,” says Dr. Hoenig. “It’s hands-on from a faculty perspective, but the student is empowered to do clinical work that day.”
Fourth-year students rotate through the clinic one day a week for the two-month semester. “By this point, they’re handling the patient care by themselves. But as a result of the earlier exposure, the cases they can see now are more complex,” she says.
Dr. Hoenig, who had 17 years of private practice experience before joining the faculty, believes that the desire to participate in patient care is a strong motivator among her students. But when schools wait until the fourth year to introduce clinical rotations, the complexity of patient care can be a shock. Students begin to see all the steps involved—communicating with the patient and referring sources, writing letters and care plans and understanding the billing. “It doesn’t matter when you start, the first time around is hard.
So the sooner you bring students into a clinical setting, the more comfortable they will be,” she says. She’s certainly sympathetic to the bewildered second- and third-year students, but she sees positive results as fourth-year students handle themselves much more adeptly because of the earlier hands-on experience. And it has also resulted in a greater interest in children’s vision and binocular vision. “We have had more interest in our residencies and in students saying they were interested in this as an emphasis of their practices.”
She adds that both the optical dispensary and the primary care clinics at the school offer a similar program of earlier exposure in a team-care learning experience. “It’s team-care, experienced faculty working with these novices so they can solve problems together.”
These initiatives represent an ongoing goal at the school and are strongly supported by the leadership at the optometry school. Dr. Hoenig also is thankful that her junior faculty colleagues have stepped up to teach less-experienced students. “This requires passion, tenacity and flexibility on their behalf as well,” she says. “I want what’s taught in my lectures to be linked to the lab. I’d like to expose them to the clinic so they can see what’s needed in the community. It’s a flow up and down. When the community demands new services, we need to teach more in the curriculum, and the trends in children’s vision and binocular vision services need to be reflected in what we offer in the clinic,” she says. That can be challenging within the framework of a university, but the process is the same as what will be required of students as young practitioners. “You have to be flexible, listen and work with all the different components to fill the need of your community.



